Abstract
Background Bias, stigmatizing language, and social isolation are significant barriers to the optimal care of pain for adolescents and young adults (AYA) with sickle cell disease (SCD). Qualitative studies that include first-person narratives of SCD pain are underrepresented in outcomes research but provide valuable information for clinical education and community care models. Here, we present the interim analysis of an ongoing thematic research study that analyzes narrative experiences of AYA patients with SCD and their journeys- both in and out of the healthcare system- with chronic pain.
Methods In this IRB-approved study, a single semi-structured interview is administered to patients ages 13-21 with sickle cell disease (Hemoglobin SS, SC, and SBeta0Thal genotypes) living in a mid-sized metropolitan center and receiving care at an academic teaching hospital. Patients are offered the opportunity to participate from inpatient units, ambulatory continuity clinics, and community advocacy groups. Interviews are conducted either in-person or remotely, recorded, transcribed, and independently checked for accuracy. The interview includes questions about coping with pain in medical and non-medical settings, interactions with the healthcare team, impacts of pain on social and community life, and opportunities to describe what patients wish family members, teachers, friends, and healthcare providers understood about living with SCD pain. Transcripts are analyzed for thematic coding by 2 independent coders using a deductive approach with latent textual analysis (Braun & Clarke, 2013). Codes are translated into themes by key-words-in-context and indigenous categorization methods (Ryan, 2011). Thematic coders are not members of the patients' clinical care teams, and patients do not provide interviews during acute pain crises.
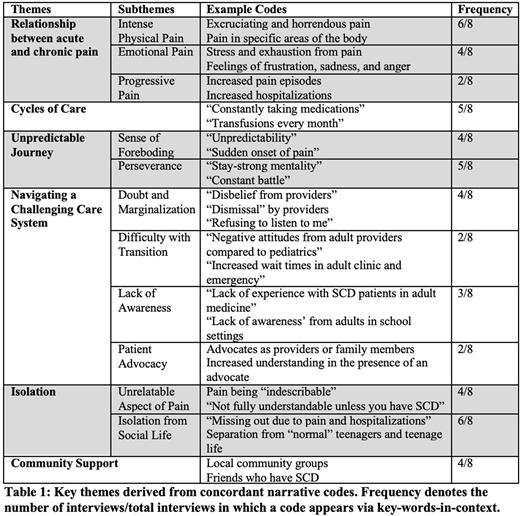
Results At the time of submission, 8 interviews were completed and analyzed. The median patient age was 17 years. Concordant coding revealed five primary themes: the relationship between acute and chronic pain, coping with rituals and cycles of care, the unpredictable nature of pain, navigating a biased healthcare system, and social isolation. The majority of patients detailed their experiences with intense, coexistent physical and emotional pain (6/8) that creates a pervasive sense of uncertainty and foreboding (4/8) in their lives. They described navigating a healthcare system that is difficult to understand, while experiencing doubts and dismissals of their pain from healthcare providers, particularly when making the transition to adult care (4/8). Lack of education and awareness about SCD in academic settings (5/8) and "missing out" on social milestones and norms (6/8) were cited as sources of isolation and emotional fatigue. Having a family member or community-based care advocate was viewed as a critical source of support within both the health system and community (4/8).
Discussion and Future Directions This ongoing qualitative research study in adolescent and young adults with SCD provides narrative data about the lived experience of sickle cell pain from the patient perspective. Interim analysis suggests several locations in the care trajectory where reports of pain may be particularly vulnerable to bias: in healthcare settings for management of acute-onset pain crisis, in schools and other academic support settings where knowledge of SCD may be incomplete, and in the transition of care from pediatric to adult care models. Particularly during acute pain management and transition care experiences, patients describe the use of stigmatizing language- in conversation and in the electronic health record- that contribute to feelings of isolation, frustration, and emotional suffering. Results of this study are being used to inform community, pastoral, and school-based sickle cell education programs as well as medical education curricula aimed at reducing stigmatizing language. Results are also being used to develop standard criteria for sickle cell patient advocates, and to improve infrastructure for the integration of patient advocates into sickle cell care teams. Future research will measure the impact of patient participation in narrative research on clinical outcomes and attitudes toward engaging the healthcare system, both for routine care and potential SCD clinical research.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.